Introduction: The Challenge of Psychiatric Documentation
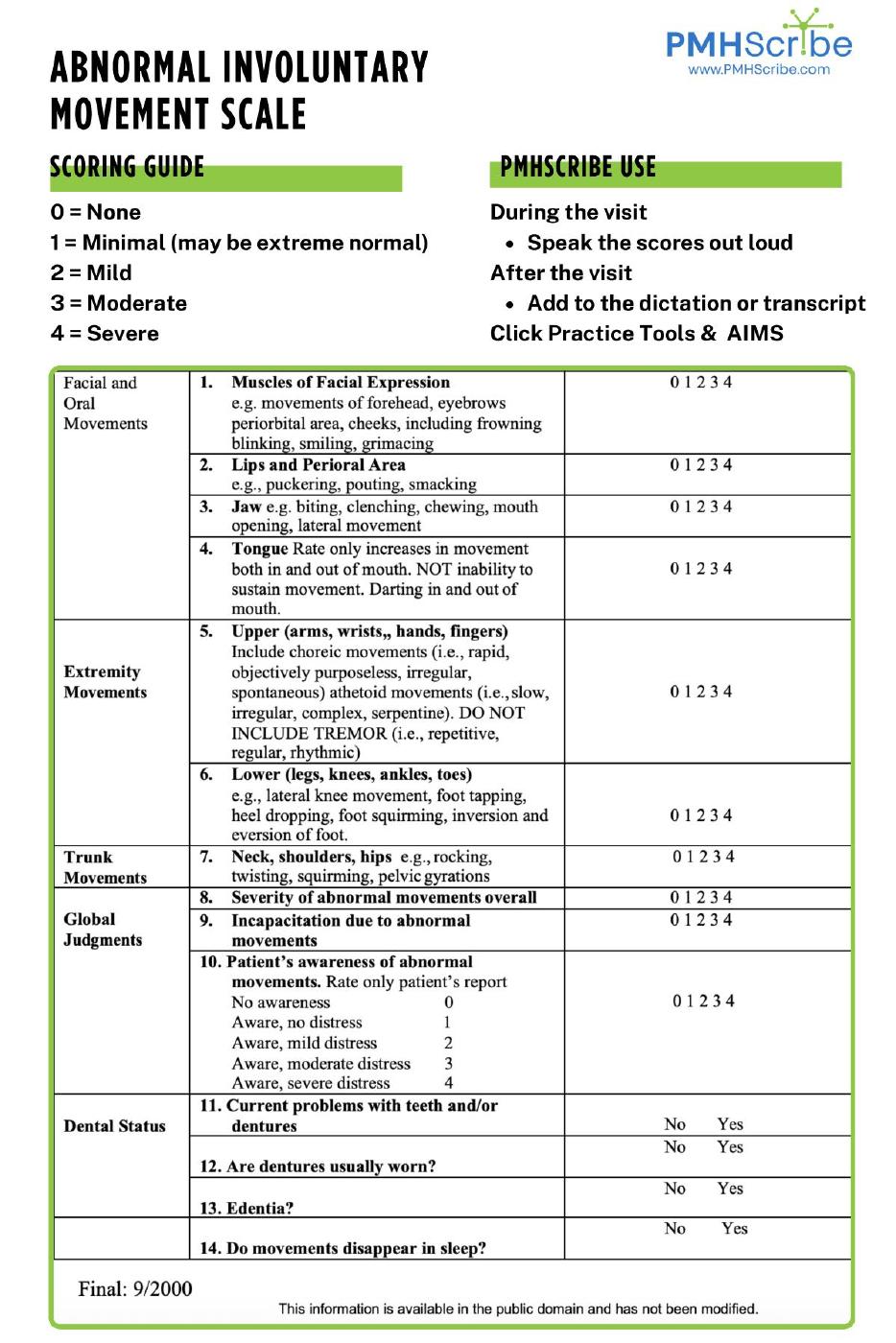
Psychiatrists, Psychiatric Nurse Practitioners, and Physician Assistants document more than symptoms. They record patient histories, side effects, treatment plans, and safety assessments. One essential tool in this process is the Abnormal Involuntary Movement Scale (AIMS), used to monitor for movement disorders related to antipsychotic medications.
Traditionally, AIMS documentation has been handled with separate forms—often printed, written on, and scanned back into the chart. This workflow interrupts the session, adds administrative tasks, and makes results harder to track across visits. PMHScribe was designed to solve this by embedding the AIMS chart directly into the psychiatric note.
The Problem With Standalone AIMS Forms
In many practices, the AIMS workflow looks like this:
- The provider fills out a separate form during the visit.
- The form is scanned and uploaded into the chart.
- Results sit in the record as an image or attachment, disconnected from the rest of the note.
This workflow creates several issues:
- Time lost in handling and uploading forms.
- Data fragmentation occurs since scanned documents are not easily searchable or comparable over time.
- Compliance risks if documentation is missing or buried in attachments.
- Patient safety concerns arise when abnormal movements are not consistently tracked.
The tool itself is sound. The problem lies in the workflow surrounding it.
What the AIMS Scale Measures
The Abnormal Involuntary Movement Scale is a 12-item clinician-administered rating system. It evaluates:
- Facial and oral movements (e.g., lip smacking, grimacing, tongue movements)
- Extremity movements (e.g., hand wringing, foot tapping)
- Trunk movements (e.g., rocking, pelvic shifts)
- Overall severity, incapacitation, and patient awareness
- Dental status, since denture problems may influence results
Each area is scored from 0 (none) to 4 (severe). The total provides a structured approach to assessing movement disorders, such as tardive dyskinesia.
When Psychiatrists Use AIMS
Best practices recommend using the AIMS chart:
- At baseline, before starting antipsychotic treatment
- At regular intervals during ongoing therapy
- When patients or families report new movements
- When medications are adjusted
Routine AIMS assessments allow providers to detect side effects early and adjust care accordingly.
Why Integration Matters
The difference between scanning a form and documenting AIMS inside the chart is significant. Integration ensures:
- Structured data – Results are stored in a way that can be trended across visits.
- Workflow efficiency – No extra steps with scanning or uploading.
- Consistency – Providers are prompted to complete AIMS at recommended intervals.
- Better patient care – Abnormal movements are easier to track, discuss, and respond to.
How PMHScribe Streamlines AIMS Documentation
PMHScribe incorporates the AIMS chart directly into its psychiatric note template. This means:
- Providers can score AIMS during the session without leaving their documentation workflow.
- Results are automatically saved within the note and available for longitudinal tracking.
- Compliance with monitoring standards is built into routine charting.
- No separate forms, uploads, or fragmented records.
By keeping AIMS within the same workflow as the rest of psychiatric documentation, PMHScribe makes it easier to deliver safe and consistent care.
FAQs About AIMS in Psychiatry
Why is the AIMS scale necessary?
It helps clinicians detect abnormal movements early, particularly tardive dyskinesia, which can become permanent if not addressed.
How often should AIMS be performed?
Most guidelines recommend every 3–6 months for patients on antipsychotics, or more often if symptoms appear.
What makes integrated AIMS better than paper forms?
Integration eliminates extra steps, keeps results searchable, and allows providers to track changes over time.
Does PMHScribe replace clinical judgment?
No. AIMS is still clinician-scored. PMHScribe ensures results are captured efficiently and consistently.
Conclusion: Psychiatry Deserves Purpose-Built Tools
The AIMS scale is central to safe antipsychotic prescribing. But when it exists outside of the chart, it creates inefficiency and risk. PMHScribe solves this by embedding the AIMS chart directly into psychiatric documentation—making assessments easier to complete, results easier to track, and care safer for patients.
Click to Download an AIMS assessment: